Introduction to the Electrocardiogram
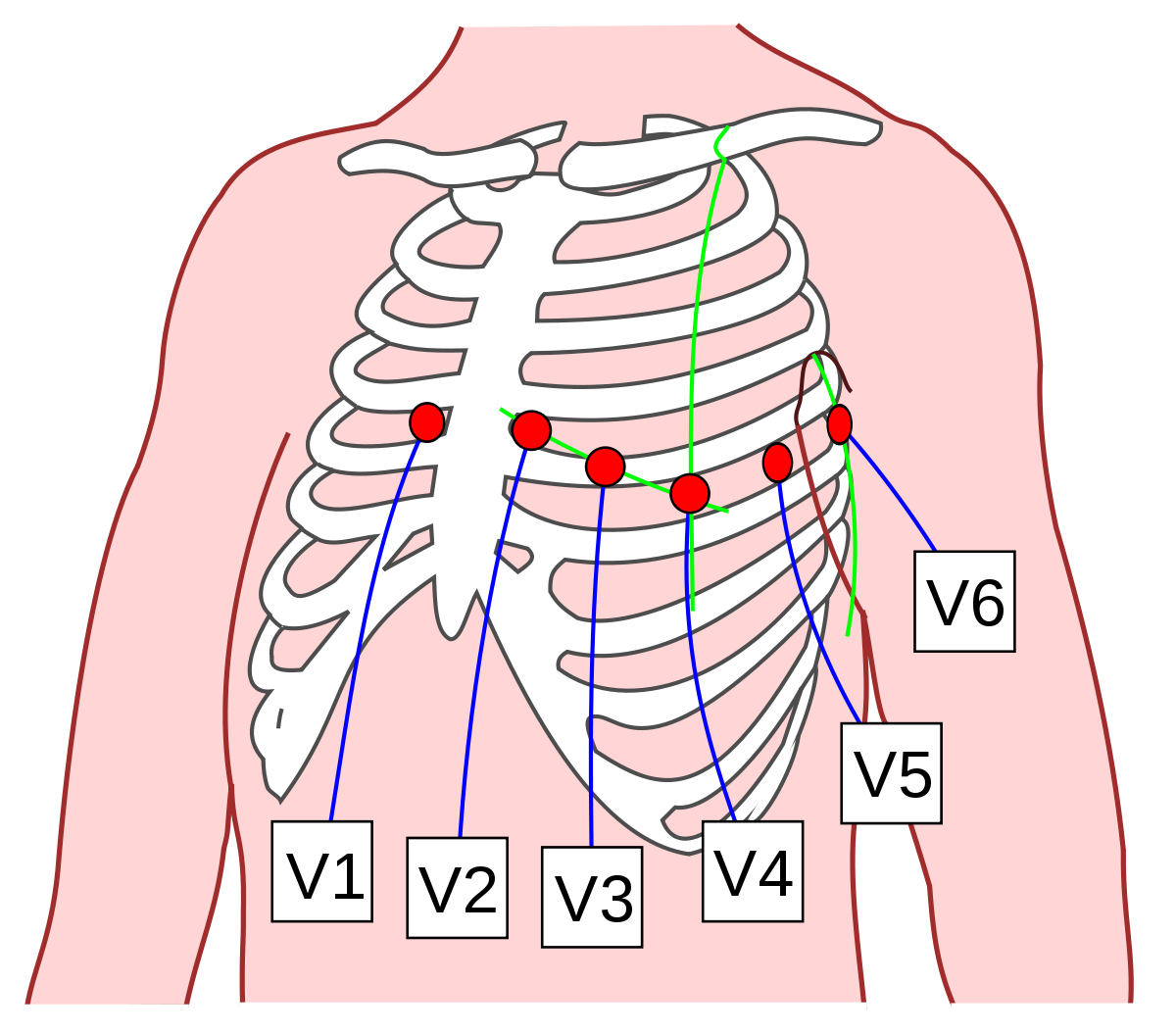
An electrocardiogram (ECG or EKG) is a test of heart function. It measures the heart's electrical activity, indicating how well each heart chamber is contracting and ejecting blood. Recall from my previous post that the heart's autorhythmic cells can generate their own action potentials which result from ion movement across cells. Ion movement results in a difference in charge across the heart, producing a potential difference. An ECG, a graph of voltage versus time, represents the combined action potentials that autorhythmic and contractile cells generate at a particular time. The action potential initiated by the heart's sinoatrial node spreads not only through the heart but also throughout the body. In an ECG, electrodes measure heart electrical activity from the chest, arms, and legs, enabling us to observe cardiac electrical activity from multiple locations. An essential point about ECG electrodes is that they do not produce or send ...




